What is a herniated disc?
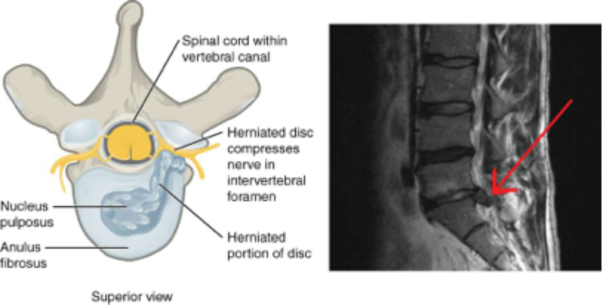 The spine is made up of a series of connected bones called "vertebrae." The disc is a combination of strong connective tissues which hold one vertebra to the next and acts as a cushion between the vertebrae. The disc is made of a tough outer layer called the "annulus fibrosus" and a gel-like center called the "nucleus pulposus." As you get older, the center of the disc may start to lose water content, making the disc less effective as a cushion. This may cause a displacement of the disc’s center (called a herniated or ruptured disc) through a crack in the outer layer. Most disc herniations occur in the bottom two discs of the lumbar spine, at and just below the waist.
The spine is made up of a series of connected bones called "vertebrae." The disc is a combination of strong connective tissues which hold one vertebra to the next and acts as a cushion between the vertebrae. The disc is made of a tough outer layer called the "annulus fibrosus" and a gel-like center called the "nucleus pulposus." As you get older, the center of the disc may start to lose water content, making the disc less effective as a cushion. This may cause a displacement of the disc’s center (called a herniated or ruptured disc) through a crack in the outer layer. Most disc herniations occur in the bottom two discs of the lumbar spine, at and just below the waist.
A herniated lumbar disc can press on the nerves in the spine and may cause pain, numbness, tingling or weakness of the leg called "sciatica." Sciatica affects about 1-2% of all people, usually between the ages of 30 and 50.
A herniated lumbar disc may also cause back pain, although back pain alone (without leg pain) can have many causes other than a herniated disc.
What treatments are available?
Most (80-90%) patients with a new or recent acute disc herniation will improve without surgery. The doctor will usually try using nonsurgical treatments for the first few weeks. If the pain still keeps you from your normal lifestyle after completing treatment, your doctor might recommend surgery. Although surgery may not return leg strength to normal, it can stop your leg from getting weaker, and relieve leg pain. Surgery is usually recommended for relief of leg pain (>90% success); surgery is less effective in relieving back pain.
Nonsurgical treatment
Your doctor may prescribe nonsurgical treatments including a short period of rest, anti-inflammatory medications to reduce the swelling, analgesic drugs to control the pain, physical therapy, exercise or epidural steroid injection therapy. If you are told to rest, follow your doctor's directions on how long to stay in bed. Too much bed rest may give you stiff joints and weak muscles, which will make it harder to do activities that could help reduce the pain. Ask your doctor whether you should continue to work while you are being treated.
Your doctor may start treatment and, with the help of a nurse or physical therapist, begin education and training about performing the activities of daily living without placing added stress on your lower back.
The goals of nonsurgical treatment are to reduce the irritation of the nerve and disc and to improve the physical condition of the patient to protect the spine and increase overall function. This can be accomplished in the majority of herniated disc patients with an organized care program that combines a number of treatment methods.
Some of the first treatments your doctor may prescribe include therapies such as ultrasound, electric stimulation, hot packs, cold packs and manual ("hands on") therapy to reduce your pain and muscle spasm, which will make it easier to start an exercise program. Traction may also provide limited pain relief for some patients. Occasionally, your doctor may ask you to wear a lumbar corset (soft, flexible back brace) at the start of treatment to relieve your back pain, although it doesn’t help heal the herniated disc. Manipulation may provide short-term relief from nonspecific low back pain, but should be avoided in most cases of herniated disc.
At first, the exercises you learn may be gentle stretches or posture changes to reduce the back pain or leg symptoms. When you have less pain, more vigorous exercises will likely be used to improve flexibility, strength, endurance and the ability to return to a more normal lifestyle. Exercise instruction should start right away and be modified as recovery progresses. Learning and continuing a home exercise and stretching program are important parts of treatment.
Medication and pain management
Medications used to control pain are called analgesics. Most pain can be treated with nonprescription medications such as aspirin, ibuprofen, naproxen or acetaminophen. If you have severe persistent pain, your doctor might prescribe narcotics for a short time. Sometimes, but not often, a doctor will prescribe muscle relaxants. However, you want to take only the medication you need because taking more doesn't help you recover faster, might cause unwanted side effects (such as constipation and drowsiness) and can result in dependency. All medication should be taken only as directed. Make sure you tell your doctor about any kind of medication you are taking, even over-the-counter drugs and supplements, and if he/she prescribes pain medication, let him/her know how it is working for you.
Nonsteroidal anti-inflammatory medications (NSAIDs) are analgesics and are also used to reduce swelling and inflammation that occur as a result of disc herniation. These include asprin, ibuprofen, naproxen and a variety of prescription drugs. If your doctor gives you anti-inflammatory medications, you should watch for side effects like stomach upset or bleeding. Chronic use of prescription or over-the-counter NSAIDs should be monitored by your physician for the development of any potential problems.
Other medications are available that also have an anti-inflammatory effect. Corticosteroid medications --- either orally or by injection --- are sometimes prescribed for more severe back and leg pain because of their very powerful anti-inflammatory effect. Corticosteroids, like NSAIDs, can have side effects. Risks and benefits of this medication should be discussed with your physician. Epidural injections or "blocks" may be recommended if you have severe leg pain. These are injections of corticosteroid into the epidural space (the area around the spinal nerves), performed by a doctor with special training in this technique. The initial injection may be followed by one or two more injections at a later date, and should be done as part of a comprehensive rehabilitation and treatment program.
Trigger point injections are injections of local anesthetics (sometimes combined with corticosteroids) directly into painful soft tissue or muscles along the spine or over the back of the pelvis. While occasionally useful for pain control, trigger point injections do not help heal a herniated lumbar disc.
Surgery
The goal of surgery is to make the herniated disc stop pressing on and irritating the nerves, causing symptoms of pain and weakness. The most common procedure is called a "discectomy" or "partial discectomy," in which part of the herniated disc is removed. In order to see the disc clearly, sometimes it is necessary to remove a small portion of the lamina, the bone behind the disc. Bone removal may be minimal (hemi-laminotomy) or more extensive (hemi-laminectomy). Some surgeons use an endoscope or microscope in some cases.
Discectomy can be done under either local, spinal or general anesthesia. The patient lies face down on the operating table, generally in a kneeling position. A small incision is made in the skin over the herniated disc and the muscles over the spine are pulled back from the bone. A small amount of bone may be removed so the surgeon can see the compressed nerve. The herniated disc and any loose pieces are removed until they are no longer pressing on the nerve. Any bone spurs (osteophytes) are also taken out to make sure that the nerve is free of pressure. Usually, there is very little bleeding.
What can I expect after surgery?
If your main symptom is leg pain (rather than low back pain), you can expect good results from surgery. Before surgery, your doctor will do an examination and tests to make sure that the herniated disc is pressing on a nerve and causing your pain. Physical examination should show a positive straight leg raise test demonstrating sciatica and possibly muscle weakness numbness or reflex changes. Additional tests can include an imaging test (magnetic resonance image [MRI], computed tomography [CT] or myelography) that clearly shows nerve compression. If these tests are all positive for you, and your doctor is sure that you have nerve compression, your chance of significant relief from leg pain after surgery is approximately 90%. Although you should not expect to be pain-free every day, you should be able to keep the pain under control and resume a fairly normal lifestyle.
Most patients will not have complications after discectomy, but it is possible you may have some bleeding, infection, tears of the protective lining of the spinal nerve roots (dura mater) or injury to the nerve. It is also possible that the disc will rupture again and cause symptoms. This occurs in about 5% of patients.
Ask your doctor for recommendations on postsurgical activity restrictions. It is usually a good idea to get out of bed and walk around immediately after recovering from anesthesia. Most patients go home within 24 hours after surgery, often later the same day. Once home, you should avoid driving, prolonged sitting, excessive lifting and bending forward for the first four weeks. Some patients will benefit from a supervised rehabilitation program after surgery. You should ask your doctor if you can use exercise to strengthen your back to prevent recurrence.
How do I know if I need emergency surgery?
Very rarely, a large disc herniation may press on the nerves which control the bladder and bowel, causing loss of bladder or bowel control. This is usually accompanied by numbness and tingling in the groin or genital area and is one of the few indications that you need surgery immediately for a herniated lumbar disc. Call your doctor at once if this happens.
